Peter G. Peterson Foundation: Almost 25% of healthcare spending is considered wasteful.
We think this is low by a factor of at least two, and here is why
Introduction
The Peter G. Peterson foundation published this report last year detailing that about 25% of your healthcare dollar is wasted. We think they are underestimating, and the real figure is over half. They contend that their plan would reap about a quarter of this back. We at Sentia think that we can get all of it back and reduce your healthcare bill by over half.
The Problem (as defined by Peterson)
Wasteful spending in healthcare is generally defined as:
- Services and processes that are either harmful or do not deliver benefits
- Excess costs that could be avoided by replacing services or products with cheaper alternatives that have identical or better benefits
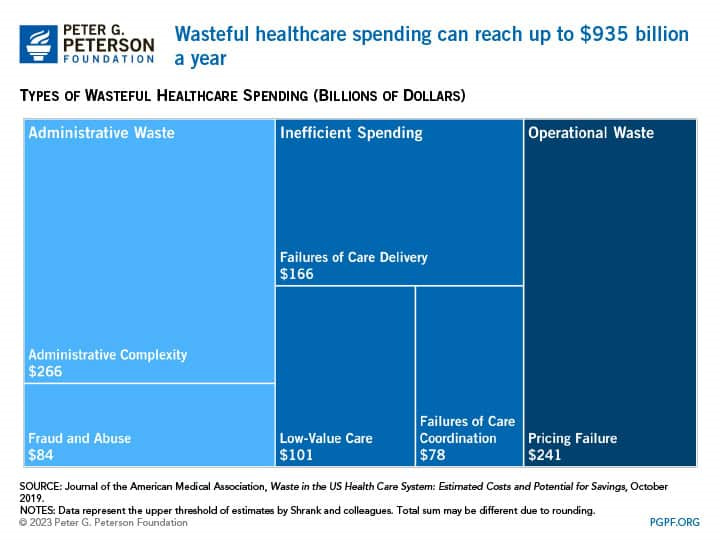
According to a 2019 study by healthcare scholars in the Journal of the American Medical Association, the annual cost of wasteful spending in healthcare has ranged from $760 billion to $935 billion in recent years, or nearly one-quarter of total healthcare spending. Such spending can generally be categorized as administrative waste, inefficient spending on clinical care, or operational waste.
Administrative Complexity
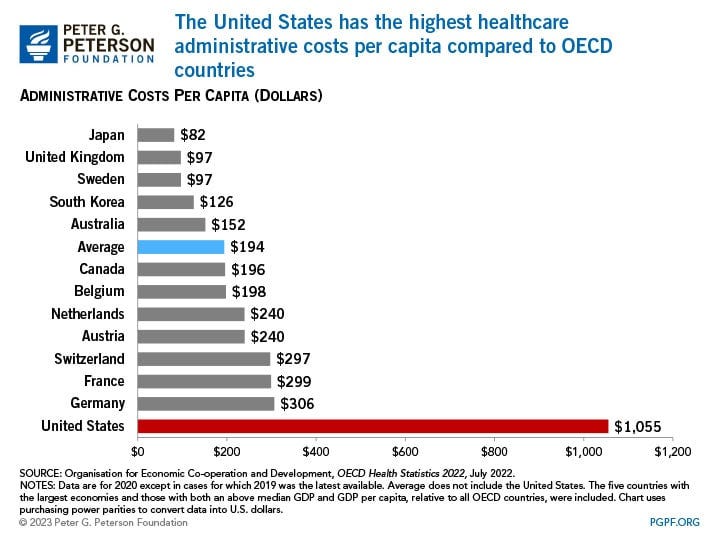
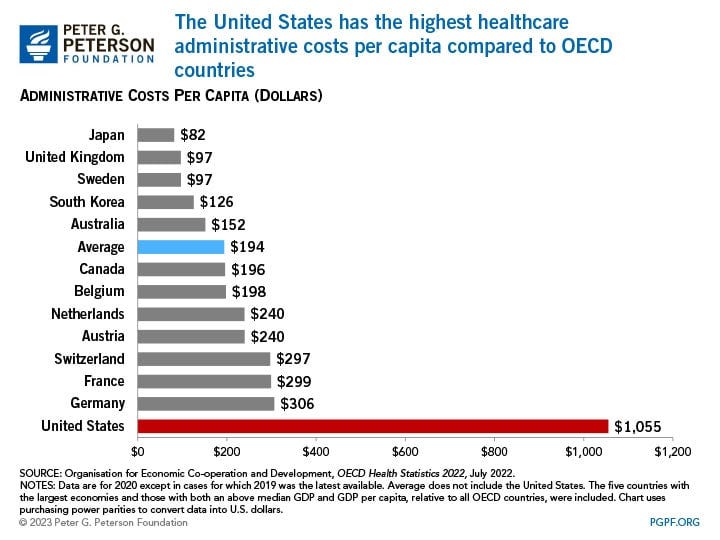
The largest source of health system waste, roughly $266 billion, is due to administrative costs. The United States spends considerably more on healthcare administration than other wealthy countries. In 2021, the United States spent $1,055 per capita on such costs, while the second highest level of such spending was Germany at $306 per capita. That difference is partially due to the administrative complexity of having multiple payers in the U.S. healthcare system, which results in higher costs associated with billing- and insurance-related expenses, including managing insurance claims, clinical documentation and coding, and prior authorization issues. That administrative complexity is illustrated by the fact that estimated time spent dealing with bill-related matters amounts to $68,000 per physician per year. However, it should be noted that much of the spending discrepancies among countries stem from the fact that the U.S. healthcare system operates differently than other OECD countries, particularly those with single-payer systems.
Pricing Failure
Operational waste is a smaller portion of wasteful healthcare spending, and it occurs in cases of pricing failure or when medical materials are misused. Pricing failure in the healthcare sector translates to inconsistent pricing of care due to different entities paying a range of prices. Prices can depend on facility setting, (e.g., inpatient versus outpatient), location (e.g., rural versus metropolitan), and type of insurance. For example, a 2021 study by the Radiological Society of North America found that the median negotiated price for an MRI scan of the lower spinal canal cost $1,311 when paid in the commercial market compared to $269 for Medicare. Pricing failure often leads to overpricing, and it affects prices for medications, payer-based health services, and laboratory-based and ambulatory services. Because the health sector operates differently than other markets, pricing failure contributes an estimated $231 billion to $241 billion of waste in the healthcare system per year; however, what is considered pricing failure by some studies may actually just be reflecting market conditions in specific areas.
Misuse of Medical Materials
The misuse of medical materials arises when less expensive but equally effective alternatives are not used or when medical materials are wasted. A common example of using less expensive alternatives is swapping out brand-name drugs for generic ones. When generics or biosimilars become available, they offer less expensive treatment options for patients and payers. In the pharmaceutical sector, waste of medical materials can manifest in large amounts of discarded and unused medicines from redundant prescriptions, patients’ non-adherence to the prescribed course of treatment, and shortcomings of hospitals’ management of drug stock. Researchers estimate that hospitals throw out $3 billion worth of medications annually.
The Real Problem
Medical loss ratio
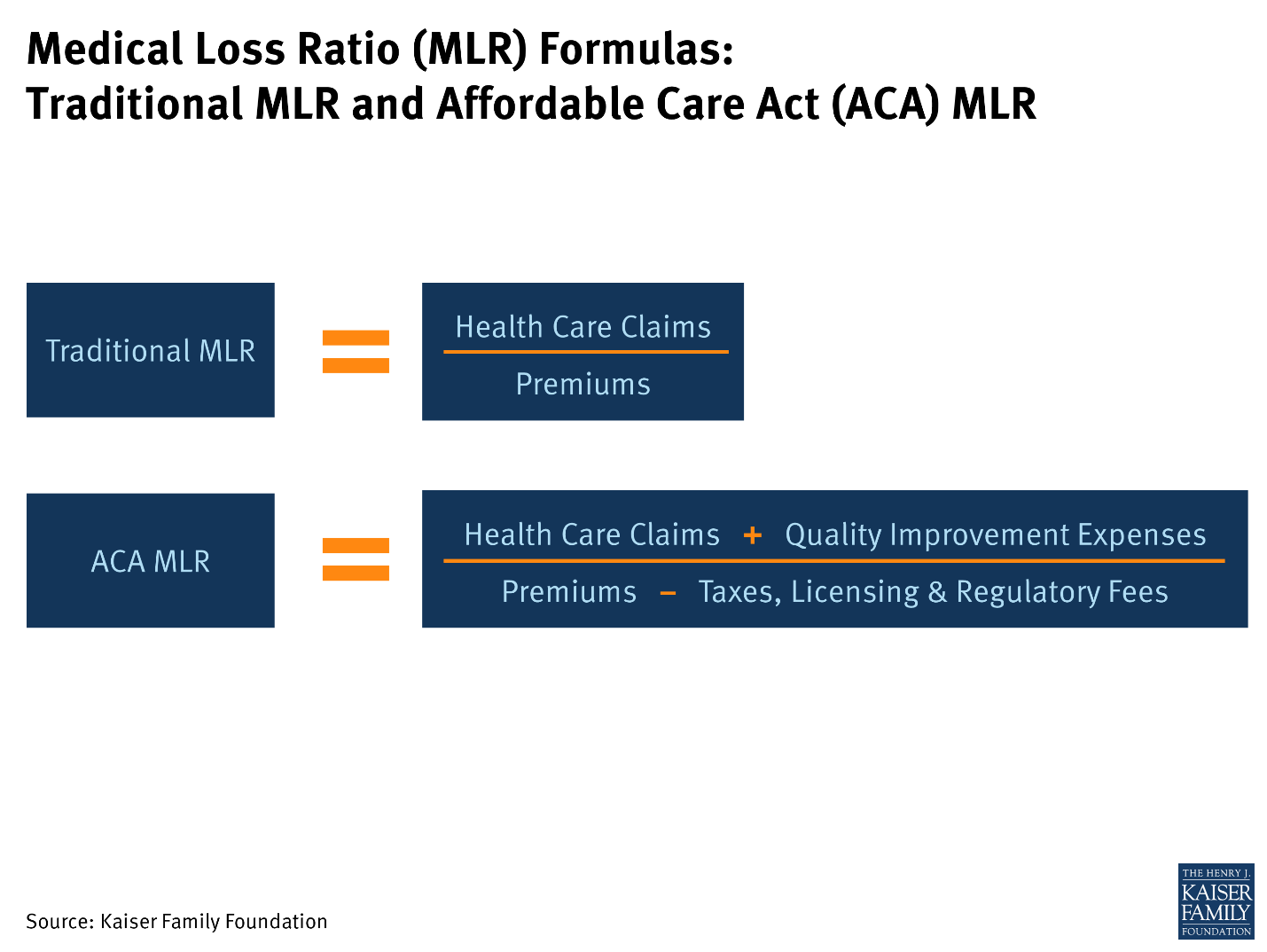
The medical loss ratio (MLR) used to be the ratio of premiums to claims. The ACA redefined MLR to include claims plus quality improvement expenses, divided by premiums minus taxes licensing and regulatory fees, like this:
While the old way of calculating was flawed at least, with only accounting for claims not payments, The new way gives huge additional loopholes. What exactly are “Quality Improvement Expenses,” how do you measure them and their effectiveness? Further, you still have the problem of claims instead of payments. Insurance companies are incentivized to deny claims and put every effort into not paying a claim, through pre-authorization, fraudulently having a doctor mark your claim as ‘medically unnecessary’ or just refusing to pay.
Our research finds that the real MLR should be payments divided by premiums is closer to 53%, that is, your insurance returns, on average, 53 cents for every dollar you pay.
Billing, Coding and Collections
In our article, “Ancillary Costs that Drive up the Bill for Healthcare,” we found that administrative costs at the individual physician level are about $66 billion per year, or $73,376 per physician. Peterson found $1055 billion and $68,000 per physician. We don't know how they arrived at this calculation, but it is clearly spurious. We used 900,000 physicians, they clearly used 15 million doctors which is obviously wrong. Statista thinks we are closer. Clearly Peterson’s numbers are incorrect.
Health and Wellness
The way we could lower healthcare costs today with no new technology, would be to manage chronic, behavior-based disease. Your insurance company could provide you with patient education based on your lab results and measurements. Then they could offer you discounts for measured, real, healthy behavior. An estimated 84 percent of health care costs are attributed to the treatment of chronic disease. If we could reduce this by even 25% we could collectively save over one trillion dollars per year out of the $4.7 trillion cost of healthcare in the US. We here at Sentia have produced this health and wellness module that integrates with your health insurance and our electronic medical record.
Pharmacy Benefits Managers (PBMs)
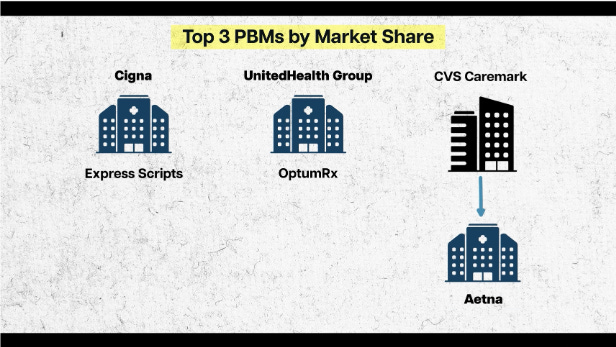
Since the Affordable Care Act was signed into law, big insurance has shifted focus from selling insurance to selling medications. There is only so much money they can hide with accounting tricks and “Quality Improvement Expenses” so they moved into the pharmaceutical market with these things they call Pharmacy Benefit Managers (PBMs). These PBMs are for the stated purpose of negotiating prices for drugs with the manufacturers, and saving everyone money. In reality, they do negotiate a better rate with the pharmaceutical companies, but instead of passing on the savings to the patient, they increase the price for maximum profits. For example, the retail price of a 4 ml. dose of Keytruda (pembrolizumab) is $6098.03, and must be administered every 3 to 6 weeks. In France you can have this drug delivered for about $91,000 per year on average. In the US, the average cost is $191,000. We have heard, but could not verify that some PBMs are charging $75,000 per dose. Since the top three PBMs are owned by big insurance, well CVS Caremark owns Aetna, but same thing, all that additional profit goes to the same old legacy insurance companies and does not count toward their 20% ACA mandated MLR.
The Real Solution
What we need is a complete rethinking of healthcare finance. Let’s take the bankers out of the works and streamline and automate all the things the insurance companies do. Here is what we have done.
- Start a new kind of insurance company that is fully automated. There is no adjudication, no denial of claims, no medical coding and no wasted administration costs
- Provide the practitioner with a fully integrated Electronic Medical Records System, (EMR). At no cost. This allows this new insurance company to detect procedures performed and pay for them, in real time
- Provide everything the practice/hospital needs to fully automate their processes as well.
- Provide the patient access to his or her medical records from anywhere in the world there is an internet connection.
- Eliminate PBMs. We can directly negotiate with the medication manufacturers exactly the same way the corrupt PBMs can, but we pass on the actual negotiated rate to the patient.
- Charge the patient the actual cost of the incurred risk plus a data administration fee of say, $10 per month.
- Provide the patient with our Health and Wellness functionality to keep them healthy and drive down costs for everyone. This program will offer discounts for actually reading and following the advice of the system, as measured by checkups and bloodwork.
That is it really. Get rid of the bankers and all the manual processes.
Conclusions
We have addressed each of the points the Peterson Foundation’s paper brought up and listed quite a number more. This indicates that the problem is far larger than they stated. We have shown a way to address each one of these problems and solve it. We have shown a way to reduce the cost of healthcare and health insurance by far more than half. Then, we will be not only the cheapest medicine in the world, but also the best. We already have the best doctors and the best equipment; we just need to implement the above detailed framework to give them all the tools necessary for success.
We have this system in prototype now, fully functioning.
Contact us here or on our site and we will be happy to provide a demonstration of the fully functional prototype.
If you liked what you read, please like and subscribe, click on the notification icon, subscribe to our newsletter, and follow us on all our social media and blog sites.
We have built a comprehensive health information system to keep the patient healthy and on the right track with the ability to incentivize healthy living. Implementing this system should be fairly simple and will completely revolutionize the way healthcare is paid for, saving countless lives. We have shown a way to use this system to make the best healthcare system in the world also the most efficacious and the most affordable, and a way to move toward value-based care.
Comment
| Date Written | Comment |
|---|